|
|
|
| Mandibular Swelling - Can It Be Multiple Myeloma? |
Ashish Gupta 1 , Pankaj Bansal 2
1 Prof and Head, Deptt Of Oral And Maxillofacial Surgery - Sudha Rustagi College Of Dental Sciences Kheri Road, Faridabad
2 Reader, Deptt Of Oral And Maxillofacial Surgery - Sudha Rustagi College Of Dental Sciences Kheri Road, Faridabad
|
| Address For Correspondence |
Dr Ashish Gupta, Prof and head
Dept of Oral Maxillofacial surgery
Sudha Rustagi College of Dental science
Kheri More,Faridabad,Haryana
Email ID:drashish71@gmail.com |
| Abstract |
| Multiple myeloma is a debilitating malignant hematological disease, characterized by multicentric proliferation of plasma cells in bone marrow. The incidence of multiple myeloma is 4.5/10,000/yr with median age at diagnosis between 63-70 yrs. Manifestation of multiple myeloma in jaw bone is not rare but involvement of mandible as first bone and diagnosis being made by oral surgeons are infrequent. Present article is about a 58 yr old female patient with the chief complain of right side facial swelling and intermittent moderate pain. Incisional biopsy revealed multiple myeloma and subsequent treatment with radiotherapy and chemotherapy followed. It stresses upon the fact that as oral surgeons / dental health professionals we may be the first one to diagnose systemic diseases in early stages. |
|
| Keywords |
| multiple myeloma ,swelling, malignant, plasma cells,incisional biopsy |
|
| Full Text |
INTRODUCTION
Multiple myeloma is a debilitating malignant hematological disease, characterized by multicentric proliferation of plasma cells in bone marrow. The incidence of multiple myeloma is 4.5/10,000/yr with median Age at diagnosis between 63-70 yrs. The mortality is 4.1/10,000/yr1.The term multiple myeloma was given by RUSTIZKY in 18732. Usually the patient presents with renal failure, bone pain, fatigue, and recurrent infections due to immunosupression.The involvement of mandible is infrequent but is even rarer to be involved as first bone. More than 30%of patients with multiple myeloma develop osteolytic lesions in jaw3at some stage of progression .The mandibular lesions are more common in the posterior region of the mandible and pain may be the only initial symptom of disease. From radiological prospective multiple myeloma can present in varied way including:
a) bone with no changes or alteration
b) multiple punched out radiolucent lesion
c) generalized bone rarefaction and osteoporotic alterations3.
The Diagnosis is based upon the evaluation of bone marrow, plasma cell infiltrate, evaluation of lytic bone lesions, detection and evaluation of monoclonal (M-) component by serum and urine protein electrophoresis1. The Present article presents the case of patient with multiple myeloma which was detected incidentally.
CASE REPORT
A 58 Yr old female patient reported in Department of Oral and Maxillofacial surgery (S.R.D.C) with the prime complain of right side facial swelling and intermittent moderate pain. Swelling was present for last 3 months and patient had earlier consulted a general surgeon who suggested them to consult an Oral Surgeon. Patient's personal family and medical histories were non contributory to her problem. There was no history of severe pain, paresthesia or loss of function. On extra oral examination, a single swelling of size approximately 3×2.5 cm involving left body region of mandible extending from premolar region anteriorly to angle region posteriorly was evident. There was no change of color of overlying skin neither there was any visible pulsation, bleeding on discharge. On palpation swelling was firm, nontender, nonpulsatile, non fluctuant with diffused margins.
Intraorally swelling size was 2.5 x 2 cm and was almost obliterating buccal sulcus. The overlying mucosa was stretched but there was still no change of color. Buccal cortex was expanded bucco lingually but more on buccal side. The OPG (fig 1)
 | Fig 1 : Opg Revealing A Well Connected Multilobular Radioluency Extending From Roght Third Molar Region To Canine Of Same Side.
 |
revealed a well connected multilobular radiolucency extending from right third molar region to canine of same side. Superioinferiorly radiolucency extended from just below upper border to 1cm above lower border dipping to height of just .5 cm above lower border in second molar region immediately anterior to angle. Margins were distinct, well demarcated, no sclerotic border present and there was no resorption of root apices seen either. Extractions were carried out in same area long back without any complications.
As a routine protocol, an incisional biopsy of lesion was planned under general anesthesia (as patient was very apprehensive), two unit of blood was administered as patient was anaemic to raise Hb levels to 10 gm %. A representative sample of tissue was taken and sent for histopathology in two different labs. Patient again reported three days after biopsy with toxic, weak and stressed out looks and high grade fever along with increased swelling of mandible. Patient was admitted immediately and managed with 3rd generation cephalosporins. In due course of time all routine and some specific investigations were conducted again. Patient's Hb came back to 8gm% and ESR was substantially raised, meanwhile histopathology reports from both labs arrived stating that sheets of malignant plasma cells showing eccentric nuclei and stippled chromatin were present suggesting plasma cell dyscrasia ( fig 2 ) .
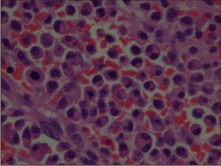 | Fig 2 : Microscopie View Showing Sheets Of Malignant Plasma Cells Showing Eccentric Nuclei And Stippled Chromatin Were Present Suggesting Plasma Cell Dyscrasia.
 |
Immediately skull and pelvic region radiographs were taken and we saw 4 to5 characteristic punched out lesions in skull (fig 3, 4).
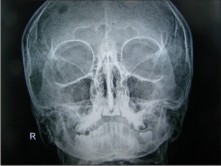 | Fig 3 : Pa View Of Skull Showing Characteristic Punched Out Lesions In Skull.
 |
 | Fig 4 : Lateral Skull Radio Graph Showing 4 To 5 Characteristic Punched Out Lesions In Skull.
 |
Patient was immediately referred to higher center where diagnosis for multiple myeloma was confirmed according to standard laid down diagnostic criteria and was advised to go for adjunctive radiotherapy and chemotherapy.
DISCUSSION
B- cell lymphoid tissue neoplasms can broadly be classified in three types
a)multiple myeloma
b) solitary plasmacytoma
c) extramedullary plasmacytoma4,5.
Multiple myeloma presents in disseminated form, in several bone while solitary bone plasmacytoma is confined to single bone. Extramedullary plasmacytomas consisting of soft tissue masses of plasma cells may occur at almost any site on the body.
Most common symptoms of multiple myeloma is bone pain specially in lumbar vertebrae region. Approximately 70% of multiple myeloma patients come with pain in bones but in present case, though intermittent, mild, vague pain was present but it was not among chief complaints .Kyle6 in his review also reported that bone pain (58%) along with fatigue related to anaemia (32%) were most common. Other systemic manifestations include pathological fracture, weight loss, fever, renal failure, diarrhea, hypercalcemia and infections. Clinical manifestations in maxillofacial region includes gingival hemorrhage, odontalgia, paresthesia, tooth mobility, migration, swelling and sometimes pathologic fractures.
Radiographically most common finding has been punched out radiolucencies without sclerotic borders. Borders are distinct but there is no definitive cortical margin. Skull lesions are present in almost 50% of patients7.It has often been described as "punched out" or en "moth eaten" appearance. Multiple investigations including complete hemogram to ascertain anemia, leukemia or thrombocytopenia is carried out .ESR too is usually elevated in these cases.
The diagnostic criterion for multiple myeloma includes;
a) presence of more than 10% of plasma cells on examination of bone marrow and monoclonal proteins in serum or urine8.
b) Detection and evaluation of monoclonal component by serum and urine protein electrophoresis, quantification of IgA, IgG, IgN immunoglobulins.
c) Evaluation of lytic bone lesions
d)Biological assessment to differentiate symptomatic and asymptomatic multiple myeloma.
Treatment has been combination use of chemotherapy and radiotherapy but in recent years preferred treatment is giving initial course of induction chemotherapy consisting of thalidomide-dexamethasone regimens and then autologous stem cell transplantation6.Although treatment is not certain in nature but it definately increases survival time.
In present case, we did an incisional biopsy keeping in mind all sorts of differential diagnosis yet it did not originally include multiple myeloma or plasma cell dyscrasia which was the diagnosis we reached eventually.
CONCLUSION
Early diagnosis of multiple myeloma is pivotal to increased survival time of patient. A thorough knowledge of maxillomandibular manifestations of multiple myeloma and other metastatic disease is a must for any dental health professional. This case emphasize that while we make differential diagnosis we should keep all factors in our mind like biochemical investigations, radiographs, clinical symptoms and we should be elaborate in diagnosis before we go for excision of any lesion. Another aspect is that we should corelate systemic condition with local symptoms. We may conclude, as incisional biopsy is important before excision of big oral lesion so is open differential diagnosis before biopsy so that we can diagnose some of fatal systemic diseases in early stage through their oral manifestations. We as oral surgeons may be helpful in diagnosing some of the systemic diseases in early stages to prevent fatal results.
REFERENCES
1. J.L.Harosseau and M.Dreyling Multiple myeloma; ESMO Clinical practice guidelines for diagnosis,treatment and follow up.Annals of oncology 21(supplement5):V155-V157,2010
2. Vieira-Leite-SequndoA,Lima-FalcaoMF,Corriea-Linis-FilhoR,Marques-SoaresMS,lopez-lopez J,Chimenos-Kustner E multiple myeloma with primary manifestations in the mandible.A case report Med Oral Patho Oral Circ Buccal 2008 April 1:13(4) :E232-4.
3. Epstein JB,Voss NJ,Stenenson-Moore P.Maxillofacial manifestations of multiple myeloma.An unusual case and review of literature.Oral surg-Oral med-Oral patho.1984 Mari 57(3):267-71.
4. Seoane J,Aguirre-Urizar JM,Esparza-Gomez G,Suarez-Cunqueiro M,Campos-Trapero J,Pomareda M.The spectrum of plasma cell neoplasia in oral pathology.Med. Oral.2003 Aug-oct,8(4):269-80
5. Canger EM,Celenk P,Alkan A,Gunhan 0.Mandibular involvement of solitary plasmacytoma:a case report .Med Oral Patol Oral Circ Bucal.2007 Jan 1 ;12(1):E7-9
6. Kyle RA,Gertz MA,Witzig TE et al. Review of 1027 patients with newly diagnosted multiple myeloma.Mayo Clin Proc 2003;78,21-33
7. Witt C, Borges AC,Klein K,Neumann HJ. Radiographic manifestations of multiple myeloma in the mandible:A retrospective study of 77 patients.J Oral Maxillofacial surg 1997 May;55(5):450-3
8. Greenberg MS,Glick M, Jonathan AS, Burket's Oral Medicine 11th edition.Ontario:B C Decker:2008 p.407-409.
|
|
|
|
|
|
|